Immunology Overview
 Immunology is the study of the immune system, which defends the body against foreign intrusion by pathogens. (right - colorized scanning electron micrograph of red blood cells - erythrocyte, platelet, leukocyte)
Immunology is the study of the immune system, which defends the body against foreign intrusion by pathogens. (right - colorized scanning electron micrograph of red blood cells - erythrocyte, platelet, leukocyte)
The immune system is intimately connected with the hematologic system since white blood cells (leukocytes, including B- and T-lymphocytes) are key players in the lymphoid system. Cellular participants in the immune and inflammatory responses include :
● phagocytic cells (dendritic cells, monocytes and macrophages, and granulocytes)
● antigen presenting cells (dendritic cells, macrophages, B lymphocytes, helper T cells)
● antibody producing cells (plasma cells)
● cytotoxic cells (CTL, NK, NKT)
● regulatory cells (APCs, helper T cells, regulatory T cells)
● cells-in-waiting (memory B cells, monocytes, naïve B cells, Tc)
● chemical releasing cells (basophils, eosinophils, neutrophils; mast cells - histamine, cytokines; hepatocytes - complement proteins)
An antigen is any molecule that stimulates an immune response. Most antigens are proteins or polysaccharides, though small molecules coupled to carrier proteins (haptens) can also be antigenic. The segment of an antigenic molecule to which its cognate antibody binds is termed an epitope or antigenic determinant. Immune responses ideally distinguish between self and other. Anergy toward self-targets operates as one self-tolerance mechanism to control the autoreactive cells found in disease-causing autoimmunity.
Immune responses are classifed as passive or active, innate or adaptive, and cellular or humoral.
These categories are not mutually exclusive. For example, both innate and adaptive immune responses employ cellular responses. Similarly, humoral and cellular responses intersect rather than being mutually independent (e.g., helper T cells assist in activation of B cells, opsonization). Unfortunately, some terminology employed in immunology predates understanding of mechanisms, so some commonly used names do not immediately reflect the distinction between cell types (NK cells versus NKT cells) or origins (lymphoid versus myeloid origins of dendritic cells). Similarly revision of chemical terminology has resulted in misleading terminology of biochemical components (e.g., complement C4b•2b was formerly termed C4b•2a).
Passive measures to prevent pathogenic incursions are provided by physical barriers to invasion – the skin, secretions, and ciliary action. Should pathogens pass beyond the physical barricade, then active innate and acquired immune reactions mount a defense.
Innate immune responses employ phagocytic cells that are circulating or tissue emplaced – granulocytes, monocytes, dendritic cells, macrophages, and B lymphocytes. The early, innate response also employs chemical responses – chemical-mediated inflammation; the complement cascade; antimicrobial peptides; and, pattern-recognition receptors (PRR), including Toll-like receptors. The innate system is considered to constitute an evolutionarily older defense strategy, and it is the predominant immune system exhibited by plants, fungi, insects, and primitive metazoa.
An induced, acquired, adaptive response begins when foreign or pathogenic substances (antigens) are 'recognized' by cells of the lymphoid system, stimulating a co-ordinated cellular/humoral response depending upon the nature of the pathogen. Antigen recognition relies on a random and highly diversified repertoire of receptors for antigens (TCR, BCR) and antigen stimulation is followed by clonal selection and expansion of cells expressing receptors with relevant specificities, accounting for immunological memory. Adaptive immune responses are typically delayed for 4 to 7 days because specific clones must expand and differentiate into effector cells before participating in host defense.
Surfaces of cells of the immune system are coated with proteins and receptors that participate in cellular signal transduction, enabling regulatory interaction:
● clusters of differentiation – a defined subset of cellular surface receptors (epitopes) on B and T lymphocytes that identify cell type and stage of differentiation, and which are recognized by antibodies.
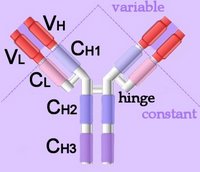
● B cell receptors (BCR) comprising one of thousands of distinct immunoglobulin superfamily molecules generated through VDJ recombination.
● T cell receptors (TCR) with heterodimers of α and β chains or γ and δ chains with Ig-like domains. Each TCR originates in a single allele and binding with a single specificity (CDR3 for antigens and CDR1-2 for MHCs).
● pattern-recognition receptors, including Toll-like receptors, which participate in the innate immune response by responding to pathogen-associated molecular patterns (PAMP) and endogenous stress signals termed danger-associated molecular patterns (DAMP).
● major histocompatibility complex (MHC) molecules of classes I, II, and III, participate in lymphocyte recognition and antigen presentation.
B lymphocytes perform the humoral immune response, and are activated when naïve B cells encounter their specific, cognate antigen. Secreted cytokines promote the proliferation of single clones of B cells that express that immunoglobulin surface receptor (BCR) which already possesses VDJ recombination-generated affinity for the antigen. Assisted by costimulation from helper T cells, B cells may undergo differentiation into plasma cells, which secrete copious quantities of the monoclonal antibody, or into memory B cells, which are primed for rapid, amplified secondary response to a repeated exposure of the priming antigen.
T lymphocytes participate in the cellular immune response, and are activated by engagement of their surface receptor (TCR), which ensures antigen specificity and MHC restriction of the response. As for B cells, costimulatory, synergistic second signaling by costimulatory molecules is also necessary to sustain and integrate TCR signaling in order to stimulate optimal T cell proliferation and differentiation. T cells include cytotoxic T cells, helper T cells, regulatory T cells, natural killer T cells, and γδ T cells.
A ф activation ф affinity maturation ф anergy ф antibodies ф antigen ф APCs ф autoimmunity B ф B cells ф basophils ф blood C ф cancer and immune system ф cancers of immune system ф CD ф cellular response ф class-switch recombination ф clonal selection ф complement system ф costimulation ф cytolysis ф cytotoxicity D ф dendritic cells E ф eosinophils ф evolution of immune and coagulation systems G ф gene conversion ф granulocytes H ф helper T cell ф hematopoiesis ф humoral immunity ф HIV/AIDs I ф immune cytokines ф immune response ф immune tolerance ф inflammatory response ф interferons ф isotype switching K ф killer T cells L ф leukocytes ф leukocyte adhesion cascade ф lymphocytes ф lymphokines ф lymphoid system M ф macrophages ф MHC ф migration ф monocytes N ф neutrophils P ф pathogens ф pattern-recognition receptors ф phagocyte ф plasma cells R ф receptors S ф secondary antibody diversification ф signaling ф somatic hypermutation, somatic mutation ф surface receptors T ф T cells ф thymus ф (tolerance) V ф vaccines ф VDJ recombination
Tables Complement Receptors Fc receptors Immune Cytokines Immunoglobulins Interferons Scavenger Receptors Toll-like Receptors Cell Adhesion Molecules Cell signaling Receptor Tyrosine Kinases (RTKs) Receptor Signal Transduction Second Messengers
tags [Immunology] [Overview]